Background:
Ibrutinib, a first-in-class Bruton's tyrosine kinase (BTK) inhibitor, has been approved for the treatment of relapsed/refractory (R/R) Mantle cell lymphoma (MCL). Both single-agent ibrutinib and combination of ibrutinib with rituximab have achieved great efficacy with manageable toxicity (Wang,NEJM2013; Wang,Lancet Oncol2015; Dreyling,Lancet2015). This study, for the first time, analyzed the real-world effectiveness and tolerability of ibrutinib for MCL patients in China.
Methods:
This multi-center, retrospective cohort study enrolled adult patients (pts) with pathologically confirmed MCL who initiated ibrutinib-containing treatment between November 2017 (date of commercialization) and April 2020. Eligible patients were retrospectively divided into 3 subgroups to receive ibrutinib-containing treatments for different purposes: R/R MCL group, newly diagnosed MCL group and maintenance therapy group. This analysis reports the baseline characteristics, efficacy and safety profiles in R/R MCL patients.
Results:
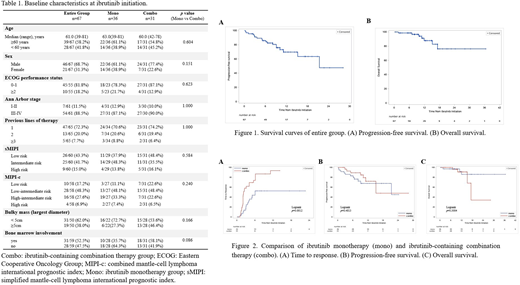
A total of 67 R/R MCL pts receiving ibrutinib-containing treatment from 9 medical centers in China were included in this analysis. At ibrutinib initiation, the median age was 61.0 (range 39-81) years, 68.7% were male and 81.8% had Eastern Cooperative Oncology Group (ECOG) performance status of 0-1. Approximately three-quarters of pts (72.3%) had 1 previous line of therapy before ibrutinib. Baseline characteristics are summarized in Table 1.
Of all patients enrolled, 53.7% (36/67) of pts received ibrutinib monotherapy and 46.3% (31/67) received ibrutinib-containing combination therapy. IR (ibrutinib and rituximab) (16/31, 51.6%) and IR2 (ibrutinib, rituximab and lenalidomide) (5/31, 16.1%) were the two most common combination regimens. Nine patients (29.0%) received ibrutinib plus R-chemotherapy. Although no statistically significant difference was found in listed baseline characteristics between these two groups, a larger percentage of pts with bone marrow involvement (58.1% vs 35.7%) and bulky mass (largest diameter) ≥5 cm (46.4% vs 27.3%) were observed in combination therapy group.
Best overall response rate (ORR) was 65.7% (20.9% complete remission [CR]). Median time to response (TTR) was 4.1 months and median duration of response (DOR) was 18.4 months. With a median follow-up of 10.2 months, median progression-free survival (PFS) was 21.3 months (95% confidence interval [CI], 15.2 - not available [NA]) (Figure 1A). PFS rates were 86.0%, 69.8% and 47.6% at 6 months, 1 year and 2 years. With a median follow-up of 11.2 months, median overall survival (OS) was not reached with OS rates of 98.5%, 87.9% and 76.3% at 6 months, 1 year and 2 years (Figure 1B). Compared with ibrutinib monotherapy, combination therapy showed higher ORR (50.0% vs 83.9%), CR rate (8.3% vs 35.5%) and shorter TTR (median TTR, 6.0 vs 2.2 months; Logrank,p=0.0012) (Figure 2A). Although the combination therapy had a trend for better PFS, no statistically significant benefit in PFS or OS was observed (Figure 2B, C).
Safety analysis focused on 55 R/R MCL pts from 3 centers with adequate adverse events information. The most common treatment emergent adverse events (TEAEs) of interest were infection (8/55, 14.6%), rash (8/55, 14.6%), bleeding (5/55, 9.1%; 1/5 was major bleeding [subdural hemorrhage]) and atrial fibrillation (3/55, 5.5%). Four pts (7.3%) experienced grade 3-4 TEAE (neutropenia, n=2; neutropenia and lung infection, n=1; subdural hemorrhage, n=1). Six pts (10.9%) had ≥1 temporary ibrutinib discontinuation due to TEAE (infection, n=3; neutropenia, n=1; rash, n=1; vomiting, n=1). One patient discontinued ibrutinib permanently due to TEAE (subdural hemorrhage). Combination therapy group showed a higher incidence of hematological TEAE (60.9% vs 39.1%) and infection (20.7% vs 7.7%). No TEAE-related death or new safety signals was recorded.
Conclusion:
This real-world analysis demonstrates that ibrutinib is effective and tolerable for R/R MCL in China. Ibrutinib-containing combination therapy outperformed ibrutinib monotherapy in response rate and TTR, but showed no survival benefits. The response rate data of ibrutinib monotherapy obtained from our study was different to existing clinical trial data, which may be mainly due to the short follow-up time of our study. Further analysis with longer follow-up is needed to validate these findings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal